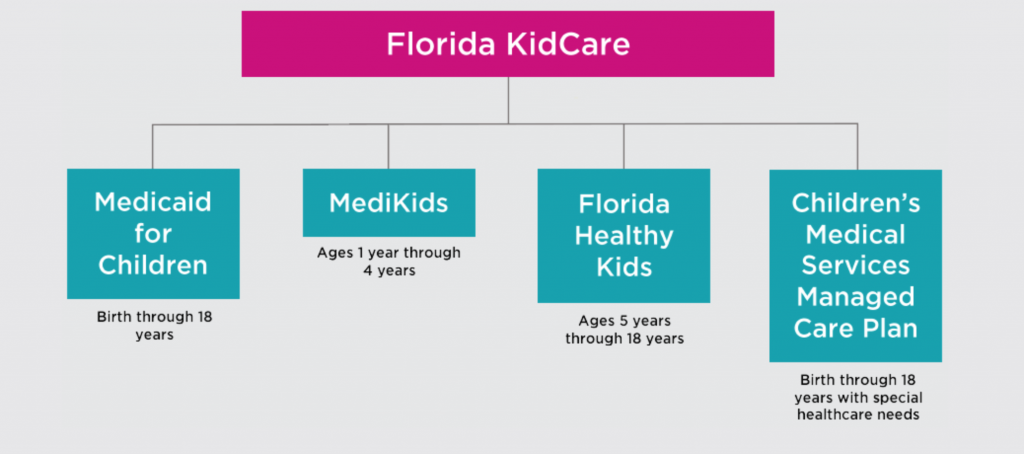
Children’s Health Care (Florida KidCare)
Florida KidCare is a single name for 4 programs which were designed to work together to ensure that children living in Florida do not go without access to healthcare — from the time they are born to when they turn 18. Which program your child fits into is generally decided by their age, your family size, and your family’s income.
These programs — Medicaid, MediKids, Florida Healthy Kids, and the Children’s Medical Services Managed Care Plan — are government-funded health insurance. Florida KidCare is made up of 4 partner organizations who oversee these programs and determine eligibility: Florida Healthy Kids Corporation (FHKC), Florida Agency for Health Care Administration (AHCA), Florida Department of Children and Families (DCF), and Florida Department of Health (DOH).
The Florida KidCare program was created through Title XXI of the Social Security Act. Florida Healthy Kids, MediKids, and the Children’s Medical Services Managed Care Plan make up the federally authorized Children’s Health Insurance Program (CHIP). The federal government creates guidelines for CHIP and gives funding to states for it, but each state implements CHIP in their own way.
If your child has had benefits or services denied or terminated by Florida KidCare or one of their partnered providers contact CLSMF for legal advice.
WHAT ARE YOUR RIGHTS?
Depending on the size of your household and family income, Florida KidCare provides free, subsidized, or full-pay options for coverage.
KidCare coverage benefits include, but are not limited to, the following:
- Doctor visits;
- Surgery;
- Prescriptions;
- Emergencies;
- Hospital stays;
- Check-ups;
- Immunizations;
- Mental health; and
- Vision and hearing.
All children who reside in Florida are eligible for KidCare, but depending on your family size and income your child’s plan may be free, subsidized, or full cost.
Children 1 year or older qualify for subsidized or full cost benefits. Subsidized plans mean that the government pays a portion of the cost and you pay any remaining amount. Children qualify for subsidized plans, which KidCare calls “premium assistance” if they:
- Are under age 19 years old;
- Are uninsured when Florida KidCare coverage begins;
- Meet income eligibility requirements (See below);
- Are a U.S. citizen or qualified non-citizen (A parent’s immigration status will never be asked.);
- Are not eligible for fully-subsidized Medicaid;
- Are not in a public institution.
Unlike other KidCare plans, children are eligible for Medicaid from the day they are born just as long as your household income is below 200 percent of the poverty level. See our Medicaid section above for program eligibility rules. While the other plans may cost as little as $15 or $20 a month, this is the only option that does not include a monthly premium fee. Medicaid also has its own premium-free Children’s Medical Services health plan, separate from the KidCare CMS plan which does charge a premium.
If you are a grandparent applying for a grandchild that lives with you, your income will only be considered if it will help your grandchildren become eligible for one of the Florida KidCare programs.
When you apply for Florida KidCare they will decide which program you are eligible for, so you do not have to research and apply to each individual program listed below.
You will need to make under a certain amount of money, depending on your family size, to be eligible for free or subsidized KidCare plans. These two resources will help you figure out whether you meet these income requirements:
The Florida KidCare annual income guidelines: https://www.floridakidcare.org/_docs/Florida_KidCare_Income_Guidelines.pdf
The Florida KidCare eligibility calculator: https://www.floridakidcare.org/calculator/
This is the only Florida KidCare option that does not require you to pay a premium, and the only option that is not considered a CHIP program.
For information about what Medicaid is and who is eligible, see our Medicaid section above.
Your child may also qualify for a CMS plan through Medicaid if they are eligible for Medicaid and have special health care needs. Continue reading for more information on CMS plans.
Children ages 1 through 4 may qualify for Florida KidCare’s MediKids program, who offers Managed Care Plans for both medical and dental insurance. MedKids is administered by the Agency for Health Care Administration.
MediKids is a CHIP program, meaning it is a state-designed program that receives federal funding.
MediKids operates through Medicaid’s Managed Medical Assistance (MMA) program and only offers enrollees Medicaid-contracted health plans.
For a list of all MediKids-covered services and the associated copayments, go to https://ahca.myflorida.com/medicaid/Policy_and_Quality/Policy/program_policy/FLKidCare/MediKids.shtml.
Your monthly premium will be decided by your family size, income, and other factors. (To check your eligibility see “Income requirements” above.)
A program providing health and dental insurance to children ages 5 through 18, Florida Healthy Kids is administered by a corporation of the same name — The Florida Healthy Kids Corporation — which has a board of directors made up of doctors, dentists, hospital representatives, advocates, and state agency representatives.
Florida Healthy Kids is a CHIP program, meaning it is a state-designed program that receives federal funding.
Your monthly premium will be decided by your family size, income, and other factors. (To check your eligibility see “Income requirements” above.)
For a list of all Florida Healthy Kids covered services and the associated copayments, go to page 29 of the Florida Healthy Kids Potential-Enrollee Guide which you can read here: https://www.healthykids.org/documents/apply/Potential-Enrollee-Guide.pdf
Your out-of-pocket costs will be limited to a maximum of 5 percent of your gross annual income (the amount you make each year before taxes and deductions are taken out). Out-of-pocket costs include copayments, and also include the monthly premium for subsidized members.
All Florida Healthy Kids insurance plans cover the same benefits but there are differences between them.
CMS plans were developed to provide quality insurance to children with special health care needs. Benefits for children enrolled in CMS include:
- A care coordinator to help the child and their family navigate the health system;
- Medically necessary, high quality services;
- Access to a wide-range of primary, specialty and facility providers throughout Florida;
- Education on preventive health services and disease management; and
- Timely processing of provider requests for service authorizations and payments.
There are two separate versions of the Children’s Medical Services plan ― one though Medicaid and the other through Florida KidCare. Both versions require that the child is eligible for the related program, is under a certain age (21 for Medicaid or 19 for KidCare), and has “special health care needs that require extensive preventive and ongoing care.” Medicaid’s CMS plan does not require a premium, while Florida KidCare’s version (a CHIP program) does.
CMS is administered by the Florida Department of Health, who has partnered with Wellcare to provide services.
Children must meet Children’s Medical Services clinical screening requirements or have a physician attest to child’s qualifying medical conditions.
Your monthly premium will be decided by your family size, income, and other factors. (To check your eligibility see “Income requirements” above.)
WHAT DO YOU NEED TO DO?
Your application for Florida KidCare is used to determine which of the four programs under its umbrella is best for you — you don’t need to fill out individual applications for each program.
To complete the online application you will need:
- Social Security Numbers (or document numbers for any legal immigrants who need insurance);
- Employer and income information for everyone in your family (for example, from pay stubs, W-2 forms, or wage and tax statements);
- Policy numbers for any current health insurance (you are allowed to apply even if you currently have health insurance from another provider);
- Information about any job-related health insurance available to your family; and
- Additional documents, if needed.
You can apply online by going to https://www.healthykids.org/application/?_ga=2.63217131.593740325.1584341680-1771500843.1584341680.
You can download an application with instructions to print out and mail at https://www.healthykids.org/apply/print/?_ga=2.43404775.316833097.1584588169-1771500843.1584341680.
You can also apply by calling Florida KidCare and following their instructions. Just call 1-888-540-KIDS (5437).
Your application may take between 4 to 6 weeks to process.
Your child will begin receiving KidCare coverage the first month after their application is processed and any required monthly premiums are paid.
Appeals of any Medicaid-related Florida KidCare programs must be done using the same appeals process listed in our Medicaid section.
Appeals of non-Medicaid Florida KidCare decisions must be made to the Florida Healthy Kids Corporation. If you feel that a KidCare decision regarding eligibility, payment, or coverage was incorrect, write a letter explaining why you think the decision was wrong (include your family’s account number) and mail or email it to Florida Healthy Kids Corporation:
- Email it to [email protected]; or
- Mail it to Florida KidCare, P.O. Box 591, Tallahassee, Florida 32302-0591.
Florida Healthy Kids will mail you a response in writing. If you are not satisfied with the result you can send a second dispute to Senior Management at the Florida Healthy Kids Corporation.
If you are still not satisfied with the result, you can send your dispute to the Agency for Health Care Administration at 2727 Mahan Drive, Tallahassee, FL 32308. You can also reach the AHCA at their toll free number: (888) 419-3456.
If you have an issue with the quality, availability, or billing of medical services your child has received you must file an appeal through your insurance plan’s provider. KidCare providers may have some differences in their appeals process but they all must conform to state guidelines set by the AHCA.
If you have had benefits or services denied or terminated by Florida KidCare or one of their partnered providers contact CLSMF for legal advice.
WHAT TO CONSIDER BEFORE TAKING ACTION?
Your child will lose eligibility for MediKids if:
- They turn 5 years old (coverage will be transferred to Florida Healthy Kids);
- They obtain other health insurance coverage;
- You don’t make the monthly payments on time;
- You don’t meet the annual eligibility renewal requirements; or
- Your child moves to another state.
You must contact your child’s primary care provider (PCP) first for medical services. If your child needs to see a specialist, the PCP must refer them. The PCP will also be able to let you know if a service is covered by MediKids. Dental issues must be handled through your dental plan provider.
You can change your child’s MediKids health care or dental plan at any time.
You can contact MediKids by phone through their helpline: 1-877-506-0578.
Your child will lose eligibility for Florida Healthy Kids if:
- They turn 19 years old;
- They are no longer a Florida resident;
- They obtain other health insurance coverage; or
- They accumulate $1 million in paid claims to Florida Healthy Kids.
You can only change insurance plans during these time periods:
- During your child’s first 90 days of enrollment; and
- During your child’s yearly renewal period.
If you dis-enroll your child from Florida Healthy Kids you may only re-enroll them at a later date if they still meet the eligibility requirement.
Your child must see a Florida Healthy Kids network provider for services, and may require a referral for their primary care provider to see a specialist.
For more information about Florida Healthy Kids’ plans and process read the Florida Healthy Kids Potential Enrollee Guide which you can find here: https://www.healthykids.org/documents/apply/Potential-Enrollee-Guide.pdf
You can contact Florida Healthy Kids by phone at 1-800-821-5437.
Along with their Managed Care Plan, CMS also offers specialty programs which are designed to focus on specific medical issues a child is facing. To read more about these programs go to http://www.floridahealth.gov/programs-and-services/childrens-health/cms-specialty-programs/index.html.
When you choose the CMS plan through KidCare you have 90 days to decide if you want to change plans or dis-enroll. After this you are “locked in” and cannot change or dis-enroll until your annual renewal period 1 year later. There are exceptions to this rule, including:
- Your child’s doctor does not, because of moral or religious obligations, provide a service your child needs;
- Your child needs related services to be done at the same time and your child’s primary care provider determines that receiving the services separately would subject your child to unnecessary risk, but not all related services are available in the plan’s network;
- Your child has an active relationship with a healthcare provider who is not in the plan’s network, but who is in the network of another subsidized plan in the area;
- The plan is no longer available in the area where your child lives;
- KidCare requires the insurance company to take action to improve quality of care; and
- Other reasons determined by KidCare, including, but not limited to, lack of access to services or providers with the appropriate experience to provide care to your child.
There are differences in the coverage and rules of the KidCare CMS plan and the Medicaid CMS plan, and this may seem confusing. To get detailed information on the plan that applies to you download the member’s handbook from one of these pages:
- Florida KidCare CMS Member’s Handbook: https://www.wellcare.com/Florida/Members/Medicaid-Plans/CMS/CMS-21
- Medicaid CMS Member’s Handbook: https://www.wellcare.com/Florida/Members/Medicaid-Plans/CMS/CMS-19
Immigrant children who lawfully reside in Florida are eligible for KidCare, and the application process never asks for the parents’ immigration status.
Prior to the passing of a law on July 1, 2016, some non-citizen children were unable to apply for KidCare until they had lawfully resided in Florida for at least 5 years. If your child was previously unable to apply due to this rule and is now eligible because the waiting period has been repealed, you can reapply online or call 1-888-540-5437.
Children who are members of federally recognized American Indian or Alaskan Native tribes may not be required to pay monthly premiums or co-payments once enrolled in Florida KidCare.
If this applies to your child, call 1-888-540-5437 to see if they are eligible for free health and dental insurance coverage.

 Home
Home